'Indian Hospitals'
Sanatoriums created to control the spread of disease like tuberculosis in Indigenous communities
Date: 1930
Sometime in the 1700s — specifically where and when is unknown — a passenger on a ship bound for North America was ill. They might have felt feverish and fatigued. They probably had a bad cough. The close confines of the vessel would have facilitated the disease’s transmission. When its passengers disembarked after their trip across the Atlantic, they had unwittingly brought with them an epidemic. Tuberculosis (TB) had arrived on the continent; by 1867, it would be the leading cause of death in the newly-confederated Canada.
This was not the first deadly disease imported from Europe. Research suggests that illness accompanied explorers as early as the 1500s. Until European contact, many Indigenous populations were widely healthy, benefitting from rounded diets and customs that promoted good hygiene. They were spared from the plagues of Europe — until, tragically, they weren’t. Many First Nations in British Columbia were decimated centuries before the arrival of Simon Fraser, one of the first Europeans to explore the mainland.
Upon reaching North America, it would take time for TB to spread to the West Coast. Even then, strides in medical research and public health were being made. By the end of the 19th century, the tubercle bacillus bacterium was isolated and determined to be an airborne contagion. Those infected, from children to the elderly, would be sent to hospitals, or sanatoria, for rest and fresh air, a treatment that remained common until an antibiotic was developed in the 1950s.
But even before the 1950s, the once-deadly epidemic was in decline across much of Canada. This wasn’t the case for Indigenous communities, though. Malnutrition and crowded conditions were common at residential schools, making them vectors for TB transmission; access to quality treatment centres was less common. Fears of interracial infection cemented existing segregation. By the 1930s, a new kind of sanatorium specifically for Indigenous people — 'Indian hospitals' — was being set up across the country, often an extension of missionary hospitals. Many grew from residential schools, and child patients would move from school to Indian hospital and then back to school: a pathological revolving door.
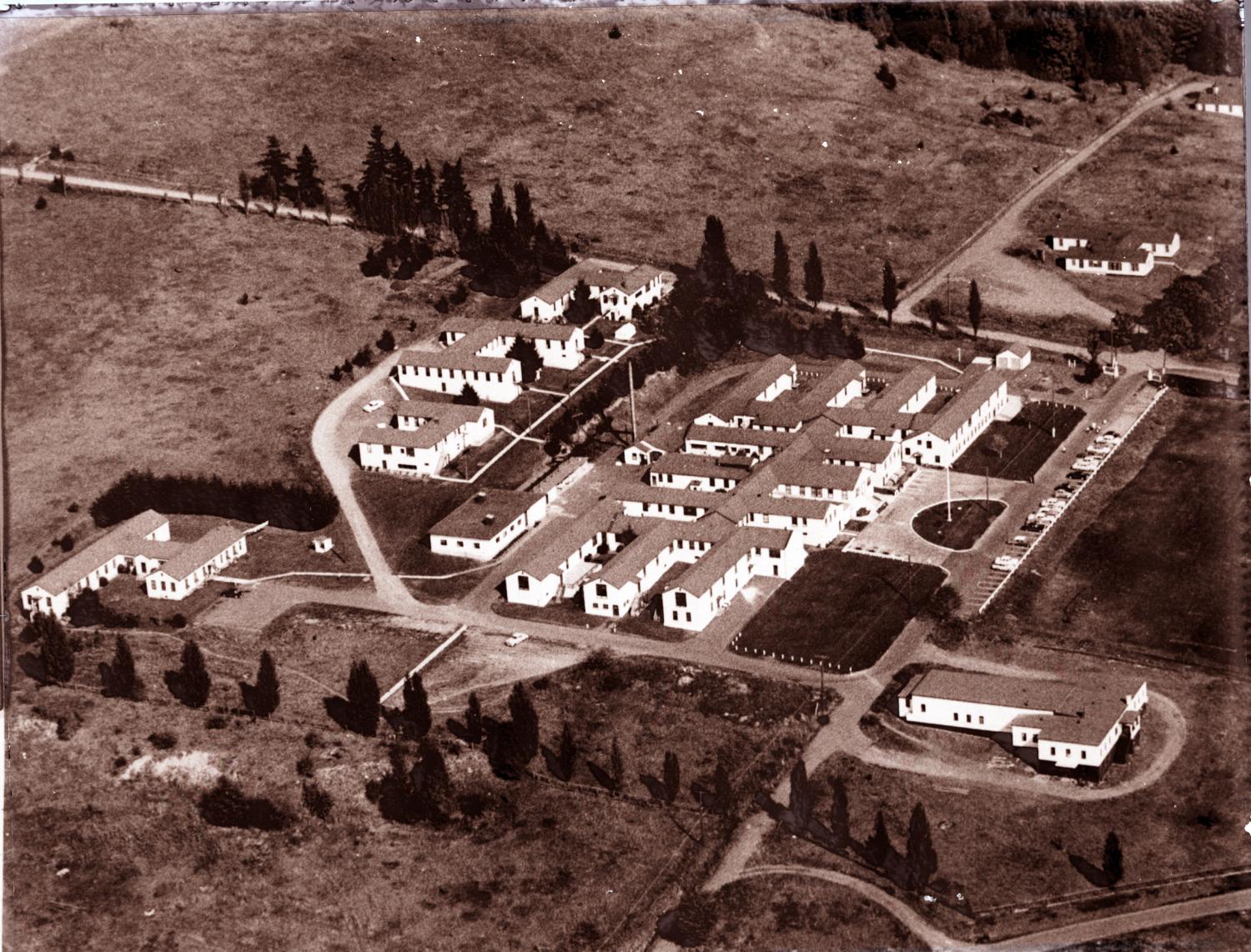
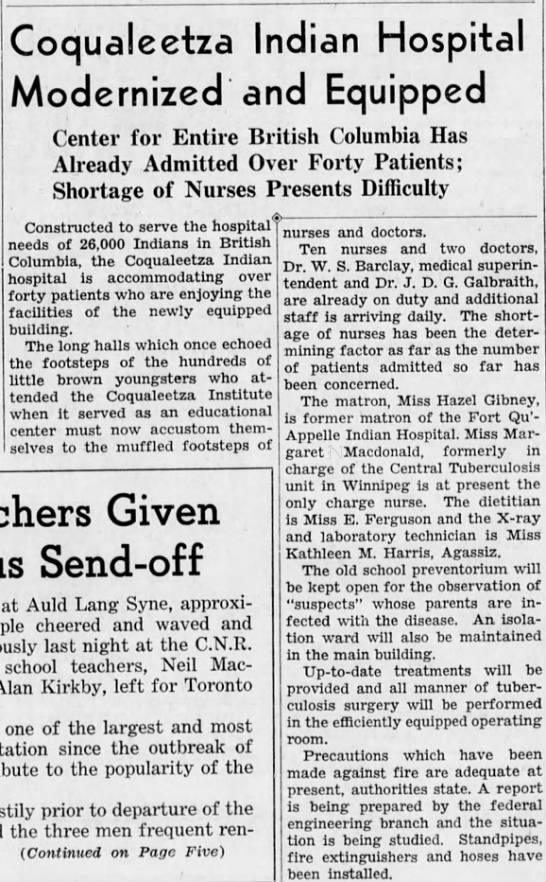
In September 1941, British Columbia’s first Indian hospital was established in Sardis, near Chilliwack. Within a decade, the Coqualeetza Indian Hospital would be followed by Miller Bay in Prince Rupert and the Nanaimo Hospital on Vancouver Island, established at the height of the system’s expansion. Conditions at the sanatoriums were abysmal — overcrowded and understaffed. The staff themselves were often undertrained and occasionally unlicensed. Painful surgeries, invasive treatments and physically restraining patients — unacceptable in general hospitals — were the norm. Sharon Whonnock, a former patient at the Nanaimo Indian Hospital, later told CBC News she spent nine years mostly strapped to a bed. "The only time we were untied was first thing in the morning to have a bath and then change our pajamas and go back to bed," she said.
In some Indian hospitals in Saskatchewan, patients were subjected to medical experimentation for vaccine development. In addition, those sent to the sanatoriums were often cut off from their communities by great distances. As a result, death rates among Indigenous patients, especially children from residential schools, were some of the highest recorded among tuberculosis patients.
As effective antibiotic treatments became more accessible in the 1950s and 1960s, TB rates in Indigenous communities began to drop. By 1971, the province’s last Indian hospital was shut down. Nevertheless, public health disparities ranging from poverty to hunger persist still today. They are reflected in how First Nations, Inuit and Métis people remain disproportionately affected by TB than other populations. In 2016, the rate of incidence in Indigenous people was nearly 40 times higher than compared to non-Indigenous people.
But things are changing. Indigenous people are one of the fastest-growing populations in Canada and are, on average, younger. Life expectancy is on the rise, as well. After centuries of tragedy, these are all signs of promise.
Sources:
1. History of Tuberculosis. Canadian Public Health Association, www.cpha.ca/history-tuberculosis.
2. Indian Hospitals in Canada. Indian Residential School History and Dialogue Centre at University of British Columbia, irshdc.ubc.ca/learn/indian-residential-schools/indian-hospitals-in-canada/.
3. Jetty, Radha. Tuberculosis among First Nations, Inuit and Métis Children and Youth in Canada: Beyond Medical Management. Canadian Paediatric Society, 14 Jan. 2020, www.cps.ca/en/documents/position/tuberculosis-among-first-nations-inuit-and-metis-children-and-youth.
4. Malone, Kelly Geraldine. Gaining Trust: History of Indigenous Experiments Poses Challenge in COVID Health. The Canadian Press, 3 Dec. 2020, www.thestar.com/news/canada/2020/12/03/gaining-trust-history-of-indigenous-experiments-poses-challenge-in-covid-health.html?rf.
5. Miller Bay Indian Hospital, 1946-1971: First Nations and Tuberculosis in Northwest BC. University of Northern British Columbia, www2.unbc.ca/sites/default/files/events/41987/public-presentation-carol-harrison-miller-bay-indian-hospital/2017-02-22-carolharrison.pdf.
6. Our History, Our Health. First Nations Health Authority, www.fnha.ca/wellness/our-history-our-health.
7. Sterritt, Angela, and Manjula Dufresne. 'Canadians Would Be Shocked': Survivors Describe Treatment at Nanaimo Indian Hospital. CBC News, 1 Feb. 2018, www.cbc.ca/news/canada/british-columbia/canadians-would-be-shocked-survivors-lawyers-describe-treatment-at-nanaimo-indian-hospital-1.4513476.
8. TB and Aboriginal People. Canadian Public Health Association, www.cpha.ca/tb-and-aboriginal-people.